We found horns on our heads and guess where else!
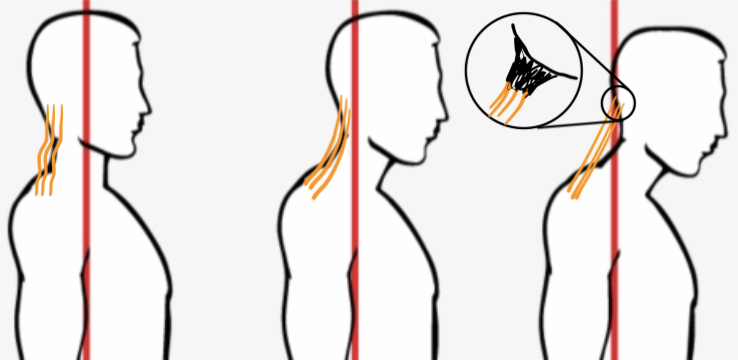
What is really going on? Is this real? Is it fake? As a downtown Seattle chiropractor, the majority of my patients are leading the world in technology so I decided to explore this claim! I looked over the past week’s head and neck x-rays. Sure enough out of the 4 out of 10 cervical x-rays taken had these “horns”. Studies claim exposure to excessive cell phone us causing the horn to grow. How is this possible? Let’s take you through the exact cause on how this happens and how to prevent it.

What is it?
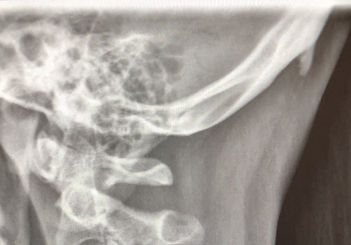
The bony horn on the back of someone’s head is called an enthesopathy; also known as insertional tendinopathy. This refers to a specific site where the ligament attaches to the bone. This “horn” forms due to the chronic pulling of tendons and ligaments on the back of the head to return the head to a neutral position. Chronic use of cell phones, tablets, computers, puts our head into a forward and down position. That’s why the Washington Post and other sources are targeting cell phones. This down-looking position of the head puts an extra strain on the back of our neck and pulls from the top of our shoulders. These muscles and ligaments act as anchors for our skull preventing it from tipping all the way forward.
Imagine the ligaments and tendons are ropes pulling an anchor out of the bone. The ligament or tendon slowly pulls away from the bone damaging the normal tissue and causing inflammation to occur. This bone eroded tissue then forms a woven pattern around the ligament or tendon protruding from the bone toward the ligament. After this woven pattern is laid down, your body lays lamellar bone fortifying the horn, creating a large spike or horn in the direction of the tendon. This commonly is explained by most physicians as a bone spur.
Where else do we have horns?
Horns or bone spurs are a result of a physiologic process called Wolff’s Law after Julius Wolff, an 1800’s experimental orthopedic surgeon. This law explains that mechanical loads can affect bone architecture. These mechanical loads come from tensile forces, compressive forces, and torsional forces.
Tensile Forces
A tensile mechanical load is most commonly seen in the bottom of the foot along the bottom of the heel protruding toward the toes. This is called a heel spur. This is caused by overstretching of the plantar fascia where it attaches to the bottom of the calcaneus bone. This is the same mechanism as the head horn.
Compressive Forces
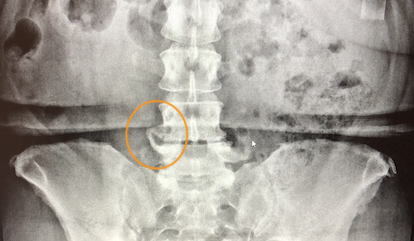
Horns or spurs occur most frequently when two bones are compressed. The most frequently compressed areas are located in the spine, hips, shoulders, and knees.
Our spine is designed with an internal shock absorber between each vertebra called a disc. When a disc is destroyed it results in less space that pushes the bones closer together adding an overload of mechanical stress to the spine. Long periods of compression lead to degeneration and spurring of the vertebral endplate. This bone on bone pressure is called degenerative disc disease and bone spurs surrounding high-stress spots.
Hips and knees are called synovial joints. This means there is a fluid capsule around the joint that lubricates the joint and provides extra cushion for compressive forces. When compressive forces constrict the knee or hip together, we see the degeneration of the joint and hip and knee. This degeneration results in pain and spurring in areas with a low concentration of joint space.

Torsional force
My favorite example of torsional stress is a baseball player. When watching a baseball pitcher we see a ball at 90+ MPH. This speed comes from the force generated through the body to release the ball at such a remarkable force. When studying bone density of baseball pitchers it is not uncommon to see higher density throughout the long bone of the arm in reaction to a twisting and torsional force. This is created by repetitive torsional forces when releasing the ball time and time again. Compare this to the opposite pitching arm and there will be quite the difference of density and strength.
How do I prevent all these stressors? See our next article for care and prevention!
References:
Hardcastle SA, Dieppe P, Gregson CL, Arden NK, Spector TD, Hart DJ, Edwards MH, Dennison EM, Cooper C, Williams M, Davey Smith G, Tobias JH. Osteophytes, enthesophytes, and high bone mass: a bone-forming triad with potential relevance in osteoarthritis. (2014) Arthritis & rheumatology (Hoboken, N.J.). 66 (9): 2429-39.
Harold M. Frost (2004) A 2003 Update of Bone Physiology and Wolff’s Law for Clinicians. The Angle Orthodontist: February 2004, Vol. 74, No. 1, pp. 3-15.
Van Der Kraan, Peter M. et al. Osteophytes: relevance and biology
Osteoarthritis and Cartilage, Volume 15, Issue 3, 237 – 244
Yochum, T. R., & Rowe, L. J. (1987). The essentials of skeletal radiology. Baltimore: Williams & Wilkins.